A habit is a tendency towards an act that has become a repeated performance, it is relatively fixed and easy to perform by an individual. We all have habits, some are beneficial to us and some we would rather do away with. For example, laying one’s bed every morning or jogging three times every week are good habits and on the other hand, smoking is a habit that is considered bad.
What are some of the habits that affect your oral health?
- Nail-biting
- Tongue thrusting
- Thumb sucking
- Mouth breathing
- Bruxism
How do they affect oral health?
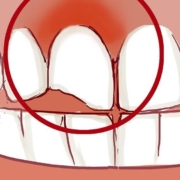
Nail-biting; nails are made of a hard material called keratin and when it is repeatedly exerted on teeth, it can cause them (especially the front teeth) to chip and eventually tip or rotate which affects how one’s smile looks.

Tongue thrusting; this involves continually pushing your tongue forward. The tongue has one of the most efficient muscle systems in the body and henceforth continued exertion of the powerful forces generated can cause the teeth position to change. This in turn affects the appearance and function of the oral tissues negatively.

Thumb-sucking; human babies resort to sucking their thumb or any other finger as a replacement or option to suckling. Beyond 5 years, however, this becomes a detrimental habit that is an indicator of deeper underlying issues. Thumb-sucking causes the teeth to be displaced anteriorly, resulting in someone having an open bite, and sometimes the lips close with difficulty.

Mouth breathing; individuals with respiratory problems especially in their early ages sometimes develop a tendency to breathe through their mouth instead of the nose. The continued mouth opening messes with the balance of the oral health structures and can lead to misalignment of teeth. It can also increase the risk of caries as the mouth is often dry.

Bruxism; this involves grinding one’s teeth and it can either be done when one’s asleep or awake and sometimes even in both states. Grinding teeth leads to attrition of the teeth where they lose part of the tooth substance and this can lead to a number of problems for example; sensitivity, malocclusion, and muscular fatigue or pain.
How can these habits be managed?
Oral habits are effectively managed when the factors that cause them are managed. This lowers the chances of recurrence or relapse.
- Most are signs of psychological stress and so a consultation with a psychiatrist would benefit some of the patients.
- In children, the use of mechanical means for example habit breakers which are designed by the orthodontist or bandaging the fingers and chemical means like applying pepper on the preferred finger can also be effective.
Treatment of the effects of oral habits is important to restore the health-related quality of life of the individual and so it is important that if one has a habit such as these, or their child has or is developing one that they seek professional help as soon as possible. It is imperative that we try to unlearn some of these habits as their effects may not be immediate but are drastic and can be expensive to reverse.